.png?width=800&auto=format)
Quality Improvement in Action: Working with Interpreters in the heart of Australia
Working with Interpreters in the heart of Australia was led by V-QIL participant, Ms Alison Thorn.
In line with NSHQS Standards Action 1.15, it is important for the diversity of consumers and high-risk groups to be considered in the planning and delivery of care and services. The team at Mental Health Services Central Australia Region, NT Health, led by Alison Thorn, undertook a project that aimed to increase interpreter use among Aboriginal clients whose first language is not English within the Subacute Facility.
Background
The Northern Territory (NT) is culturally and linguistically diverse. Aboriginal people account for approximately 30% of the NT population and experience a higher burden of disease. Aboriginal people comprise 70% of hospital admissions and 72% of service occasions at health centres in the NT. There are more than 100 Aboriginal languages and dialects spoken. NT Health staff are also culturally and linguistically diverse. Previous research has identified the low uptake of Aboriginal interpreters in health care in the NT.
Project Summary
The aim of the project was to increase interpreter use in Mental Health Services Central Australia Region. The goal was to offer 100% of Aboriginal clients at the Subacute Facility, whose first language is not English, an Aboriginal interpreter by November 2022.
Using interpreters when working with culturally and linguistically diverse clients is best practice. Subacute is an 8 bed step up, step down Mental Health residential facility in Alice Springs. There have been extensive Mental Health Quality Improvement (QI) and Aboriginal Cultural Safety Projects undertaken in previous years. However, the use of Aboriginal interpreters remains low. The project was inspired by cultural safety and working with interpreters being identified as a Mental Health Strategic Priority area.
The Northern Territory (NT) is culturally and linguistically diverse. Aboriginal people account for approximately 30% of the NT population and experience a higher burden of disease. Aboriginal people comprise 70% of hospital admissions and 72% of service occasions at health centres in the NT. There are more than 100 Aboriginal languages and dialects spoken. NT Health staff are also culturally and linguistically diverse. Previous research has identified the low uptake of Aboriginal interpreters in health care in the NT.
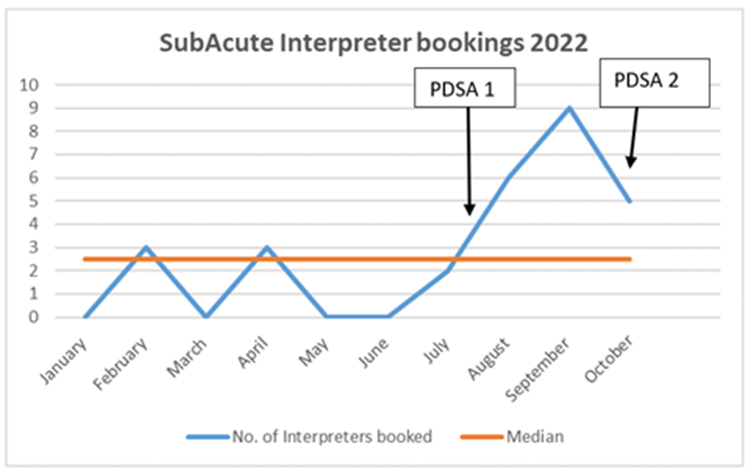
Data from Mental Health interpreter booking logs was collected from January 2022 at baseline and monthly until October 2022 after interventions. The data log included the number of Aboriginal interpreters booked per month. Qualitative data of staff feedback from training sessions was also collected.
Brainstorming workshops were held with the Subacute nursing and medical staff to identify barriers for clients accessing interpreters. The steps involved in booking interpreters was process mapped to identify any gaps that could be addressed. Suggestions that arose from brainstorming sessions were tested in 2 PDSA cycles. The initial cycle included reviewing the process for booking Interpreters in addition to developing and refining the process map. The second cycle was re-implementation of the Working with Interpreter Training (WWIT) for the Mental Health service.
As these improvements become more established it is hoped Aboriginal interpreters will continue to be booked for clients at the Subacute Facility to improve mental health outcomes. The Aboriginal Interpreter Service was not included as a key stakeholder, however their engagement in future would enhance the impact of the project.
Results
Run charts (Appendix 1) demonstrate that as a result of these interventions the number of Aboriginal interpreter bookings per month doubled over all PDSA cycles. Qualitative data indicated that overall staff felt positive about the WWIT, as it was helpful and informative.
If improvement is sustained though ongoing PDSA cycles, the project could augment existing Mental Health QI projects, inform local guidelines, and support the development of an orientation package for staff. If successful, the project could be expanded to other areas within Mental Health Services in Central Australia and the Barkly regions.
Credits: Alison Thorn, Nurse Education Coordinator, Mental Health Services Central Australia Region, NT Health
Want to engage in a real life project to improve patient quality and safety?
Our recent V-QIL Program participants at NT Health show how QI tools can be used to improve health equity and outcomes among diverse population groups across NT.
This project is an example of the invaluable knowledge, experience and practical insight that is developed on the Virtual Quality Improvement Lead (VQIL) Training Program. This nine-month program is led by an expert faculty and is an investment in your career. Throughout the course you will be supported through interactive sessions, project work and assessments.
The Improvement Academy offers V-QIL training to individuals or a group within an organisation based on the specific service provider. To learn more, click here.
“It was great to learn about QI science and the QI tools available to use in the clinical setting to look at system issues to solve problems. The modules were interactive and it was a great opportunity to network with other colleagues in the NT, rather than work in silos. Great course- would highly recommend.”
- Ms Alison Thorn, Nurse Education Coordinator, Mental Health Services Central Australia Region, NT Health
Project References
ACSQHC [Internet]. Australian Charter of Healthcare Rights; c2022 [cited 2022 Oct 27] from: https://www.safetyandquality.gov.au/
Centre for Culture, Ethnicity & Health [Internet]. Assessing the need for an interpreter; c2020 [cited 2022 Nov 24]. Available from https://www.ceh.org.au/
Harrison BT, Rubin G. PDSA QI Cycle. Clinical Practice Improvement- Diagnostics. 2021: ACHS Improvement Academy (PowerPoint slide. 6).
Mithen V, Kerrigan V, Dhurrkay G, Morgan T, Keilor N, Castillon C, Hefler M, Ralph AP. Aboriginal patient and interpreter perspectives on the delivery of culturally safe hospital-based care. Health Promotion Journal Australia. 2021 32 (1):155-165.
NSW Health Department [Internet]. Easy Guide to Clinical Practice Improvement A GUIDE FOR HEALTHCARE PROFESSIONALS ; c2002 [cited 2022 Nov 24]. Available from https://www.health.nsw.gov.au/
Northern Territory Health. Aboriginal Interpreter Policy Guideline NT Health; 2017
Paul, K. Interpreters as Voice for Patients with Limited English Proficiency. MedSurg Nursing. 2022 31(4): 247-252.
Ralph A, Lowell A, Murphy J. et al. Low uptake of Aboriginal interpreters in healthcare: exploration of current use in Australia’s Northern Territory. BMC Health. 2017 17 (733).
United States Environmental Protection Agency [Internet]. Lean Thinking and Methods- Kaizen; c2022 [cited 2022 Nov 28]. Available from https://www.epa.gov/
Woll A, Quick KK, Mazzwei C, Selameab T, Miller JL. Working With Interpreters as a Team in Health Care (WITH Care) Curriculum Tool Kit for Oral Health Professions. MedEdPORTAL. 2020 10894 (16).

